Employee Member Resources

New Member Resources
Are you new to Capital Health Plan? Review our resource page designed for new members, where you can find a new member checklist, resource guide on available CHP services, tools, and programs, and learn about important first steps as a new CHP member.
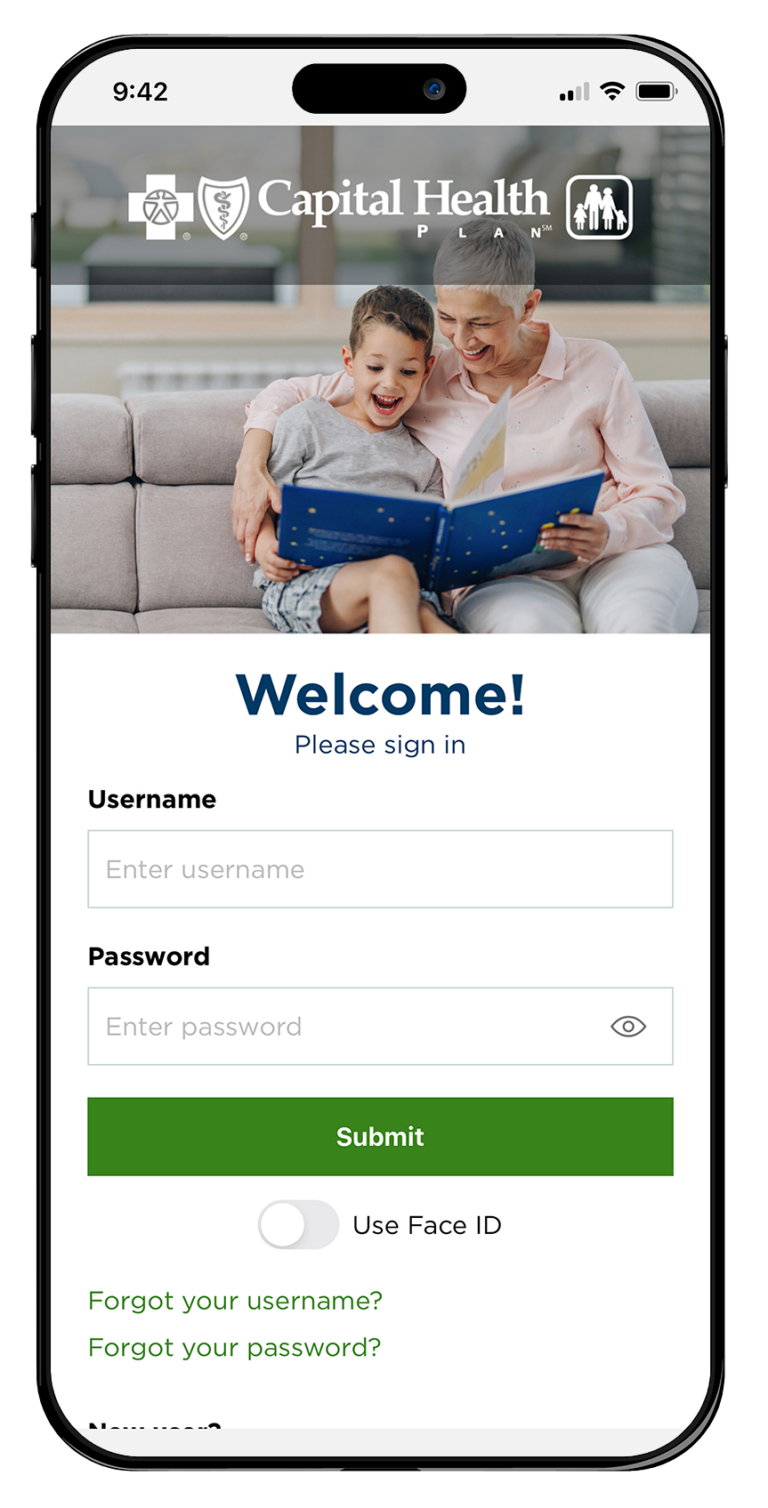
CHPConnect
The online tools available through CHPConnect provides members with quick access to the health plan information they need.
- Search providers or choose a PCP
- Access benefit documents and claims
- Review referrals and authorizations
- Review lab results and health records
- Request ID cards
Plan Benefits
CHP members can explore their plan’s specific Summary of Benefits (SOB), prescription coverage, and drug formulary, as well as find additional information and forms.
Available Health Care Services
CHP plan members have access to a variety of health care services, tools, and programs to enhance their well-being.
Pharmacies, Medications & Immunizations
Pharmacy Services
Medication Center
Immunizations
Keeping You & Your Family Healthy With CHP’s Healthwise®
Stay Current With CHP
Serving our communities with key healthcare trends, expert medical perspective, and patient-centered events.
The Latest CHP News
Gall Bladder Health
Keep your Heart Healthy
Resolve to be Healthier
Weight Management: 5 steps to weight loss
More Important Information
Table of Contents
Out of Network Coverage
Learn about Capital Health Plan’s out of network coverage for CHP members who may be traveling outside of our service area.
Get Out of Network Care
Away From Home Care
Community Resources
Find information on community resources available for those who need assistance inclusive of food insecurity assistance, mental health services, transportation services, and more.
Referrals & Authorizations
Understand the difference between a referral and an authorization, and how to obtain each one from your primary care physician or specialist for certain services.
Learn More About Referrals & Authorizations
Appointment of Representatives Forms & Instructions
Looking to appoint a relative, friend, advocate, attorney, or your physician to act as your representative? CHP members can find and complete a specialized form here.
Download an Appointment Representative Form
Determinations, Grievances & Appeals, and Utilization Management
You have a right to request medical care or services, payment for medical services received, exceptions and redeterminations, and file appeals or grievances, in addition to understanding how Capital Health Plan makes health care decisions.
Transition Process
Sometimes you are taking a drug that is not on our formulary and have to obtain a temporary supply of the prescribed medicine. It is in your best interest to learn about the drug transition process and next steps for obtaining your medication.
Request a Temporary Drug Supply
Member Rights & Privacy Notice
CHP Members are entitled to certain rights and responsibilities. Click here learn more about member rights and responsibilities. Our CHP members have a right to privacy and confidentiality for their nonpublic personal, financial, and health records. To understand how we use your personal information and how we protect your information, please review Capital Health Plan’s Member Privacy Notice.
Forms
Authorization to Disclose Protected Health Information Form
Communication Directive Form
Wellness Reimbursement Form
Health Terms Glossary
Our Health Terms Glossary was created to help you understand exactly what each service, treatment, program, diagnosis, and commonly used medical term means.
Frequently Asked Questions
The Physician Group of Capital Health Plan provides comprehensive health care exclusively for Capital Health Plan members. Their goal is to promote disease prevention and healthy living, so in addition to diagnosing and treating illnesses, they also provide preventive care, health risk assessments, immunizations, screening tests, comprehensive management of chronic conditions, and education on maintaining a healthy lifestyle. You can learn about what services are offered in the Physician Group of Capital Health Plan at any time.
Yes, all care services must be performed by a network physician or facility, unless a prior authorization has been completed in advanced, if you are traveling and out of the service area, or in the case of an emergency.
The Non-Medicare Prescription Drug Reimbursement Form should be used when requesting reimbursement for prescription drugs. Reimbursement requests can take up to 30 days for processing and may take longer if additional information is needed. You may also contact CHP Member Services for more information.
Your benefit documents are available on the CHPConnect portal. You can either request your Summary of Benefits & Coverage information from your benefits administrator, or access your Large or Small Group Summary of Benefits & Coverage Form online, or on CHPConnect.
Prefer to talk to a real person?
Get your questions answered. Contact our Member Services team.
Capital Health Plan Silver Advantage (HMO), Advantage Plus (HMO), Preferred Advantage (HMO), and Retiree Advantage (HMO) are HMO plans with a Medicare contract. Enrollment in Capital Health Plan Silver Advantage, Advantage Plus, Preferred Advantage, and Retiree Advantage depends on contract renewal. This information is not a complete description of benefits. Contact the plan for more information. Limitations, copayments, and restrictions may apply. Benefits, premiums, and/or copayments/coinsurance may change on January 1 of each year. The formulary, pharmacy network, and/or provider network may change at any time. You will receive notice when necessary.
If you have questions, please call Member Services at (850) 523-7441 or 1 (877) 247-6512 8:00 a.m. – 8:00 p.m., seven days a week, October 1 – March 31; 8:00 a.m. – 8:00 p.m., Monday – Friday, April 1 – September 30. State of Florida members call 1 (877) 392-1532, 7:00 a.m. – 7:00 p.m. TTY/TTD (850) 383-3534 or 1 (877) 870-8943.